Poster 16 - Lisa Bearpark, Thoracic Surgery
MMK Department's Day 2024
Lisa Bearpark, Thoracic Surgery
Title: Implications of Pacemaker Implantation Following Aortic Valve Surgery for Endocarditis: a SWEDEHEART Study
Scientific Summary
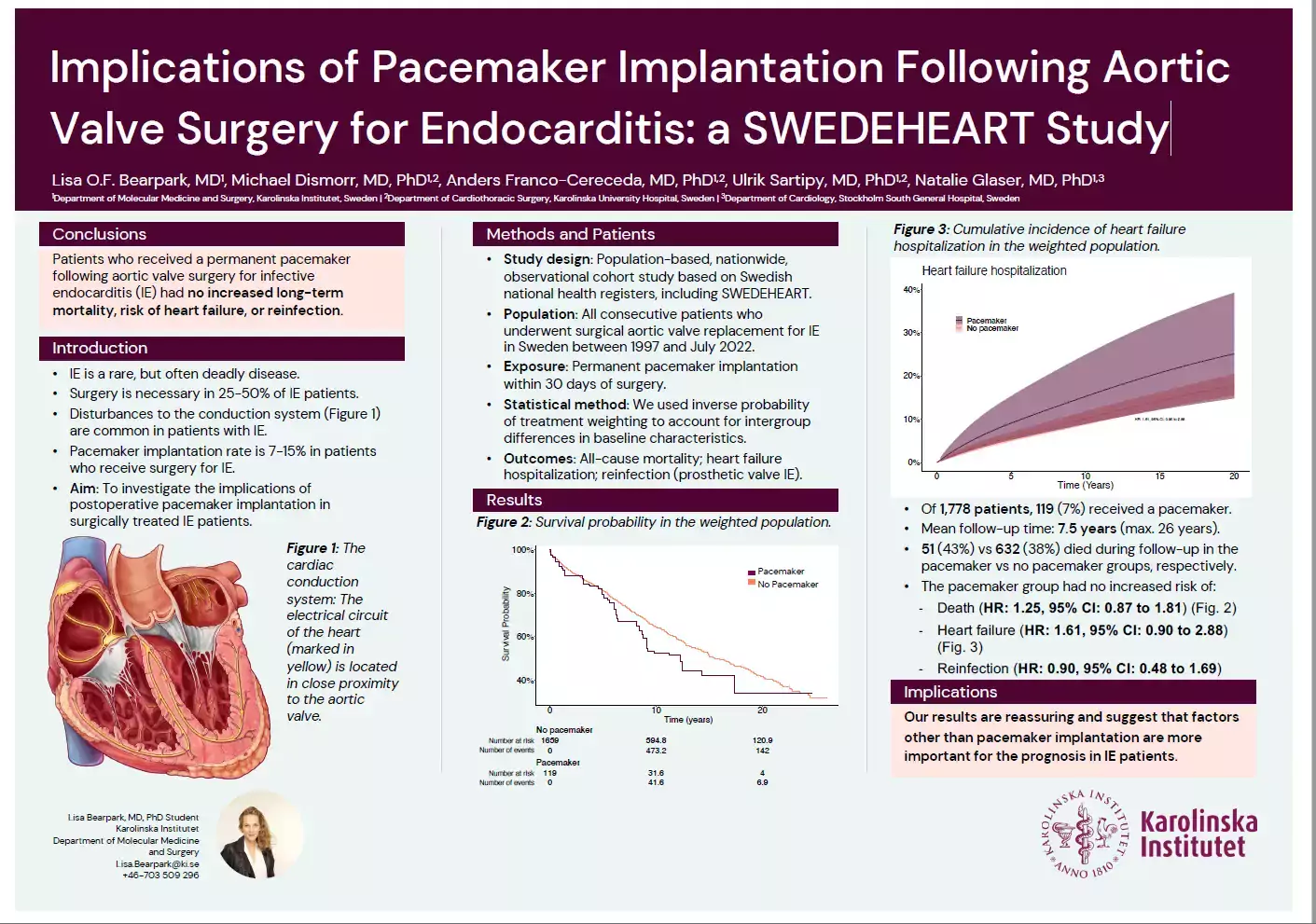
Background Infective endocarditis (IE) is associated with a high risk of heart block and surgery adds to the risk of receiving a permanent pacemaker. The clinical impact of pacemaker implantation in IE patients needs further study. We analyzed the risk of mortality, heart failure hospitalization, and prosthetic valve endocarditis in patients who received a permanent pacemaker within 30 days of aortic valve surgery for IE.
Methods In this population-based, observational cohort study, based on the SWEDEHEART register, we included all patients who underwent primary valve replacement for native aortic valve IE in Sweden 1997-2022. Outcomes were all-cause mortality, heart failure, and prosthetic valve endocarditis. Inverse probability of treatment weighting was used to account for intergroup differences. Flexible parametric models were used to estimate hazards and cumulative incidences.
Results Among 1778 patients, 119 (7%) received a permanent pacemaker. The mean age was 58 years; 335 (19%) were female. During a mean follow-up time of 8.5 years (maximum 26 years), 683 patients (38%) died. At 20 years, the cumulative incidence of all-cause mortality in the pacemaker versus the no pacemaker group, respectively, was 66% versus 59%. For heart failure hospitalization, it was 25% versus 18%. After adjustment, we found no risk difference during follow up in mortality (HR 1.25, 95% CI: 0.87-1.81), heart failure (HR 1.61, 95% CI: 0.9-2.88), or reinfection (HR 0.90, 95% CI: 0.48-1.69) in the pacemaker group compared with the no pacemaker group.
Conclusions Permanent pacemaker implantation after valve surgery for native aortic valve IE carried no increased long-term risk of death, heart failure, or reinfection. These results are reassuring and suggest that factors other than pacemaker implantation are more important for the long-term prognosis in IE patients.
